PharmSmart: Catch me if you can! Management of DYSPNEA!
By AccentCare“I can’t catch my breath!” How often  do we hear this from a patient with an advanced illness? Dyspnea, defined as an uncomfortable abnormal awareness of breathing, is one of the most common symptoms experienced by patients at the end of life. Not only is it uncomfortable for the patient, but it’s difficult for the family and caregivers to observe. However, dyspnea can occur at any stage of a debilitating disease. It's essential to understand how it may happen, how it presents, its underlying etiology, and, most importantly, how to treat it.
do we hear this from a patient with an advanced illness? Dyspnea, defined as an uncomfortable abnormal awareness of breathing, is one of the most common symptoms experienced by patients at the end of life. Not only is it uncomfortable for the patient, but it’s difficult for the family and caregivers to observe. However, dyspnea can occur at any stage of a debilitating disease. It's essential to understand how it may happen, how it presents, its underlying etiology, and, most importantly, how to treat it.
What’s the pathophysiology of dyspnea?
Dyspnea is characterized by the underlying etiology and feeling of air hunger, there is an increase in the respiratory drive leading to increase ventilator demand. Because there may also be some form of obstruction or restrictive lung disease occurring, there is a decrease in ventilator capacity and pulmonary compliance. The bidirectional signals transmitted from the motor cortex to the sensory cortex and outgoing motor command to the ventilator muscles lead to a chain of command of chest wall tightness, back to the brain stem, and to the sensory cortex.
What are the common symptoms or presentation of dyspnea?
A WHOLE lot of breathlessness including (but not limited to):
- Rapid breathing (tachypnea)
- Excessive breathing (hyperpnoea)
- Hyperventilation
- Shortness of breath
- Chest tightness
- Palpitations
- Wheezing
- Coughing
- Pain
- Fatigue
Moving forward with the management and treatment of dyspnea, a comprehensive assessment must be conducted to identify any underlying diagnosis or etiologies that may be causing the problem. Some example questions to start off, when did the patient's symptoms start? Do the symptoms occur suddenly or only when an offending factor is involved? What makes the symptoms worse or better? How long do the symptoms occur, or is it constant? These probing questions may lead to appropriate tests to be conducted to identify an underlying chronic illness and appropriately correct hypoxemia.
Suggested diagnostic tests include the following, generally earlier in the disease process:
- Arterial blood gas to determine the patient’s respiratory acid-base status
- Pulse oximetry to evaluate for hypoxia
- Chest radiography to discover any physical findings for suspected pulmonary origin
- Complete blood count and electrolytes including renal and hepatic function tests to evaluate for anemia, polycythemia, leukocytosis, or neutropenia which may assist in diagnosis
- Spirometry to detect airflow obstruction
The next table provides some examples of diagnoses that dyspnea may occur in some disorders.
| Origin | Diagnoses |
| Respiratory | • Asthma • COPD • Pneumonia • Pulmonary embolism • Lung malignancy |
| Neuromuscular or Psychogenic | • Spinal cord dysfunction • Chest trauma with fracture • Myopathy and neuropathy • Phrenic nerve paralysis |
| Cardiovascular | • Congestive heart failure • Pulmonary edema • Acute coronary syndrome • Pulmonary hypertension • Cardiac arrhythmia • Valvular heart defect |
| Other Systemic Illnesses | • Anemia • Acute renal failure • Cirrhosis • Sepsis • Anaphylaxis • Angioedema |
The treatment of dyspnea should begin by correcting the underlying cause of symptoms. For example, with respiratory disorders such as asthma or chronic obstructive pulmonary disease (COPD), there is an increase in airflow resistance with bronchoconstriction. Clinicians can utilize disease-modifying therapies to optimize the management of COPD and asthma. Treatments with inhaled bronchodilators and corticosteroids have provided some improvement in symptoms and reduce dyspnea. The following table lists the primary steps in the management of dyspnea.
| Identifying underlying etiology | Perform comprehensive dyspnea assessment including physical, emotional, social, and spiritual aspects of symptoms |
| Address reversible contributors | Treat underlying cause to improve physical function |
| Treat symptomatically | Utilize non-pharmacological and pharmacological interventions |
What are non-pharmacological interventions to treat dyspnea?
A WHOLE host of multidisciplinary regimens (but not limited to):
- Pulmonary rehabilitation
- Patient education of the psychosocial-spiritual impact of dyspnea-anxiety cycle
- Energy conservation techniques
- Cognitive-behavioral therapy
- Relaxation techniques
- Gait aids
- Acupuncture
- Fan/Medical air
- Oxygen and therapeutic room air
Now, what are the pharmacological interventions to treat dyspnea?
OPIOIDS! Opioids are the first-line pharmacological treatment option for symptomatic refractory dyspnea. There are many formulations available for patients with complex diet orders and difficulty swallowing. Opioids can be possible by mouth (tablet or solution), intravenous injection, subcutaneous injection, and probably rectal administration. Giving the opioid by inhalation seems like it would be ideal, but this route of administration has led to poorer results and is not recommended. The mechanism of action is unclear, but research suggests a reduction in sensitivity to hypercapnia and hypoxia. Opioid selection and dosing will be dependent on the pharmacokinetics and patient characteristics. The following chart will provide an overview of opioids, including pharmacokinetics and clinical pearls, to consider for patients with organ dysfunction.
| Drug | Onset | Peak | Duration | Clinical Pearls |
| Morphine |
PO: 15 min |
PO: 1.5-2 hrs |
PO: 4 hrs |
• Histamine release: Decreases BP, itching • Dose adjust or avoid in renal impairment |
| Hydrocodone |
PO: 60 min |
PO: 2 hrs |
PO: 4-6 hrs |
• Caution with PRN orders due to acetaminophen component |
| Oxycodone |
PO: 15-30 min |
PO: 1-2 hrs |
PO: 4-6 hrs |
• Safer in renal dysfunction |
| Hydromorphone |
PO: 30 min |
PO: 60 min |
PO: 4-6 hrs |
• High potency, more euphoria • Slightly safer in renal dysfunction |
| Fentanyl |
IV: 1-2 min |
IV: 5 min |
IV: 1-2 hrs |
• Safe in renal and liver dysfunction |
Wow! That's quite a list! What about side effects – well we all know there's a risk with using opioids. If used correctly and safely, it can be beneficial to treat patients with refractory dyspnea. Let's consider the common side effects associated with opioid therapy:
- Central Nervous System (CNS) depression – it is essential to counsel patients on CNS depression, which may affect their mental and physical alertness. Especially patients with fall risk, it is imperative to allow patients to see how they may feel on the first few doses before they begin their normal daily activities.
- Constipation – Consider preventative measures such as co-prescribing opioids with stimulant laxatives; increase fiber and use of osmotic laxatives to reduce the risk of constipation.
- Respiratory depression – as a Black Box Warning, respiratory depression is a severe or life-threatening fatal risk. Counseling patients to be closely monitored, especially during initiation and dose escalation. Some symptoms to observe are slow or shallow breathing, daytime sleepiness, bluish-colored lips, fingers or toes, or depression.
- Less common side effects include hypotension, anaphylaxis and allergy (if patient has a hypersensitivity reaction to other phenanthrene-derivative opioid such as codeine, hydromorphone, oxycodone, or oxymorphone), gastrointestinal, hematologic, neurologic, and dermatologic effects.
The significant drug interactions we should pay attention to with opioids and increase risk of CNS depression are as follows:
- Concomitant benzodiazepine or CNS depressant
- Alcohol
- Concomitant opioid agonists
- Cannabis or related type products
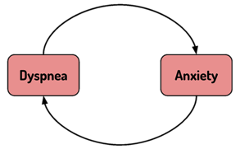
Opioids remain first-line pharmacotherapy options for dyspnea, and benzodiazepines should never be used as first-line monotherapy. A Cochrane systemic review found no benefit for benzodiazepine use for chronic dyspnea and found its use was associated with an increase in mortality risk when used with opioids. However, benzodiazepine may be considered for patients with concomitant anxiety with dyspnea. Air hunger or shortness of breath often leads to anxiety, which can compromise or worsen respiratory status by increasing respiratory demand and decrease pulmonary compliance. Some clinicians have co-prescribed benzodiazepines for patients with refractory anxiety and dyspnea. It is just crucial to be VERY cautious when starting both agents at the same time!
Bottom-line it for me! How would you approach a patient presenting with dyspnea?
- Dyspnea is the sensation of uncomfortable or difficulty breathing
- Determine the root cause of the dyspnea whether it is reversible and use disease-modifying treatment strategies
- First line of pharmacotherapy for dyspnea is opioids
- Opioid for dyspnea require lower doses than for pain and titrate to lowest effective dose
- Supplemental oxygen has only shown benefit in patients with hypoxia
Ok, let's get real with a patient case. Mr. Cookie is a 73-year-old male with atrial fibrillation on warfarin, hyperlipidemia, and end-stage chronic obstructive pulmonary disease (COPD) who presents to the emergency department with shortness of breath, wheezing, and progressive fatigue over the past 7 days despite utilizing disease directed treatment. You begin to start thinking of the next best treatment plan for Mr. Cookie.
What is the next step in Mr. Cookie’s treatment plan?
- Begin goals of care discussion and immediately refer the patient to hospice
- Start low dose morphine
- Assess for anxiety and start low dose lorazepam
- Perform further assessment to determine if underlying etiology exists
Oh no, poor Mr. Cookie! Let's consider – looking at Mr. Cookie's extensive past medical history may prompt further investigation. So choice (A) is not a great choice because there may be reversible causes to help Mr. Cookie's symptoms. And although opioids are first-line therapy and low dose morphine may be considered for Mr. Cookie's pharmacological treatment of symptomatic dyspnea, choice (D) is the best choice! During diagnosis, it's essential to perform a comprehensive physical, mental assessment to consider if there is an underlying etiology to address, including anxiety. Therefore, choice C is not the best choice for Mr. Cookie's treatment plan.
Let’s consider a few LAST multiple-choice questions for the road!
- Which is considered as first-line pharmacotherapy for dyspnea?
- Inhaled corticosteroids
- Opioids
- Benzodiazepines
- Anticholinergics
- Which of the following are respiratory patterns of dyspnea? Select all that apply.
- ↑ ventilatory demand
- ↑ ventilatory capacity
- ↑ airway resistance
- ↓ pulmonary compliance
- Which of the following are TRUE regarding the management of dyspnea in advanced illness?
- Educate patient this is an expected symptom at the end-of-life
- Utilize non-pharmacological and pharmacological interventions to treat refractory dyspnea
- Most opioids will reduce the sensation of dyspnea
- Morphine is frequently used to treat dyspnea, but is not the best choice in advanced renal disease
- All of the above are correct
Answers:
- B
- A, C, D
- E
PharmSmart is a monthly article dedicated to best practices in drug management for patients nearing the end of life, with a little cheer and lightheartedness woven throughout. It is edited by Dr. Mary Lynn McPherson, PharmD. Dr. McPherson is the Executive Director of Advanced Post-Graduate Education in Palliative Care at University of Maryland. Dr. McPherson is a consultant pharmacist to Seasons, and answers complex medication questions for our clinical teams at all hours of the day or night. She is a nationally-recognized expert in medication management for hospice and palliative care patients.
This edition of PharmSmart was written by Cindy Nguyen, PharmD.